Prior authorization requirements can hold up the fulfillment of a specialty prescription by an average of 5-10 business days. Medications requiring prior authorization will only be covered by insurance payers if the prescriber requests and receives approval from the patient’s health insurance company or pharmacy benefit manager (PBM).
These requirements are especially prevalent for specialty therapies. Specialty drugs are often prescribed for complex or chronic medical conditions and rare diseases. They also are often high cost, have complex methods of administration or require special shipping and handling. The patients receiving these medications also stand to benefit the most from quick access to their prescribed therapies due to the nature of their disease state.
The process for completing prior authorizations using manual methods—via paper and fax machines—can be inefficient and time-consuming, preventing healthcare providers from focusing on what matters most: patient care. While this is a well-known challenge in the specialty pharmaceutical space, fax machines are still a fixture in many medical offices. Healthcare providers often rely on them for their guarantee of HIPAA-compliant information exchange. Fortunately, there is a HIPAA-compliant alternative to the fax that can prevent therapy initiation delays caused by antiquated tools and processes.
1. Electronic prior authorization improves speed to therapy
Leveraging e-prior authorization solutions can improve prior authorization processing time from days to minutes. Through advanced benefit verification tools, digital platforms can pull comprehensive patient coverage results that include prior authorization requirements. Prepopulated questions and response options for the appropriate prior authorization request can be pulled based on a combination of the product and patient’s insurance coverage. Prior authorization determinations for some therapies can be returned in as little as one minute with connectivity for real-time e-prior authorization submission for more than 80% of payer-covered lives.
2. Real-time e-prior authorization reduces administrative burden
Paper-based prior authorization forms often result in missing, inaccurate or incomplete information that leads to administrative rework and calls back and forth between the pharmacy, payers and healthcare providers. The American Medical Association reported in 2017 that 75% of physicians say the burden associated with prior authorization is “high” or “extremely high” and 22% of physicians reported that they or their staff spend more than 20 hours a week completing prior authorization requests.
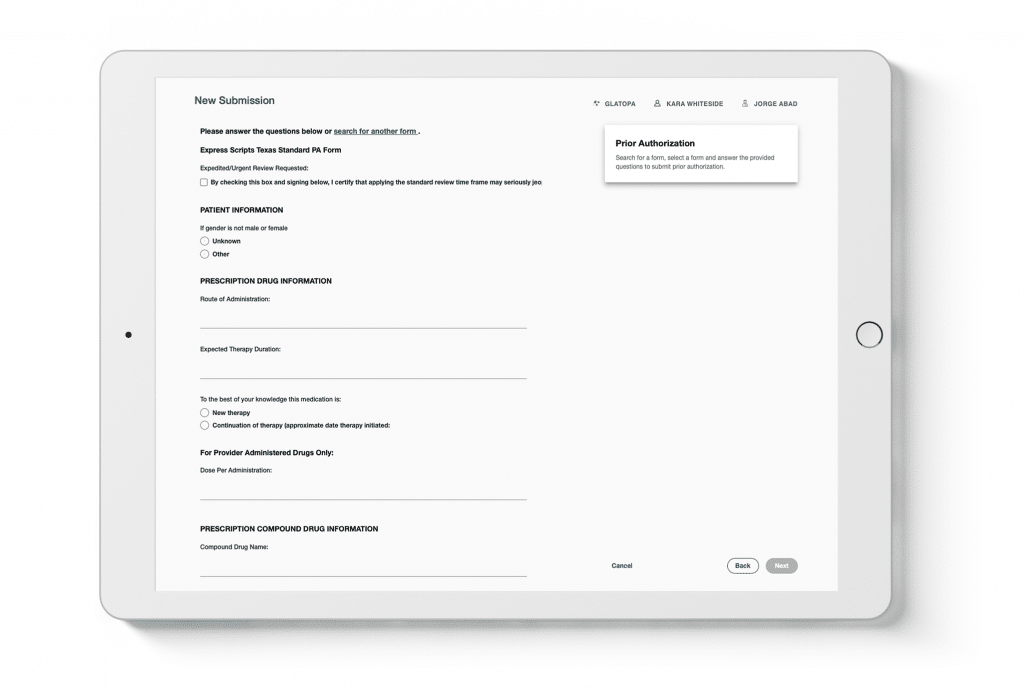
With real-time e-prior authorization tools, healthcare providers can prospectively complete a prior authorization with prepopulated questions and response options for the appropriate prior authorization request based on a combination of the product and the patient’s insurance coverage. Determinations using these tools can be returned in as little as a minute, allowing staff to spend more time with patients and reduce phone calls, paperwork and faxes.
3. HIPAA-compliant, automated tools improve efficiency
The fax machine is a long-recognized HIPAA-compliant method of transmitting protected health information (PHI). Therefore, many healthcare providers rely on this tool, even as other industries have abandoned it. Submitting prior authorizations electronically using iAssist is as HIPAA compliant and secure as using a fax machine, and provides automation that drastically improves office efficiency.
4. Gain transparency into e-prior authorization statuses
When prior authorizations are submitted electronically, it is much easier to track approvals, rejections, requests for more information and other needs from the payer in real time. This transparency allows healthcare providers to take any necessary steps to move the prior authorization through the process. Additionally, for many prior authorizations, determinations can be made in minutes, which can help the healthcare provider take the next steps required to get the patient onto therapy in the same session.
Electronic prior authorization ensures patients take the right medication
Consistently denied prescriptions and lengthy prior authorization submission processes can cause concern for healthcare providers. Afterall, healthcare providers want to be sure that their patient can gain access to a certain therapy and in a timely manner. By offering quicker, less burdensome prior authorization processes in real time at the point of care, patients are more likely to start on their prescribed therapy. The faster a patient can me moved to therapy initiation, the more likely they are to adhere to their treatment.
5. Electronic prior authorization increases adherence
As stated above, primary adherence rates are directly impacted by how quickly the patient is able to receive their medication from the pharmacy. When the prior authorization process is reduced to same-day approval in many cases, patients are more likely to get their prescription filled, especially when the process is accompanied by cost transparency at the point of care.
Improve your practice’s office efficiency with iAssist and its real-time electronic prior authorization tool
Real-time prior authorization with iAssist guides you through an automated process for submitting prior authorizations, improving processing time from days to minutes.
Leveraging connections with e-prior authorization service providers such as Surescripts Electronic Prior Authorization tool and other payer and PBM connections, our Real-time Electronic Prior Authorization tool presents pre-populated questions and response options to simplify the process and provides rapid response times on approvals.
With iAssist, healthcare provider offices can eliminate paper-based prior authorization forms that often include missing, inaccurate or incomplete information that result in follow-up phone calls and time-consuming rework.